Ushur for Provider Service
Elevate the Health Plan Provider Experience
Empower provider service teams with domain-specific AI Agents that understand complex payer systems and deliver timely, compliant resolutions at scale.

Context‑aware guidance
Connects benefits, claims and credentialing data to resolve provider needs across the end-to-end journey.
Scalable, 24×7 support
Handles surges and after-hours demand automatically without disrupting service quality.
Compliance & security
Meets HIPAA, HITRUST and healthcare standards with built-in data protection guardrails.
Adaptable & Accessible
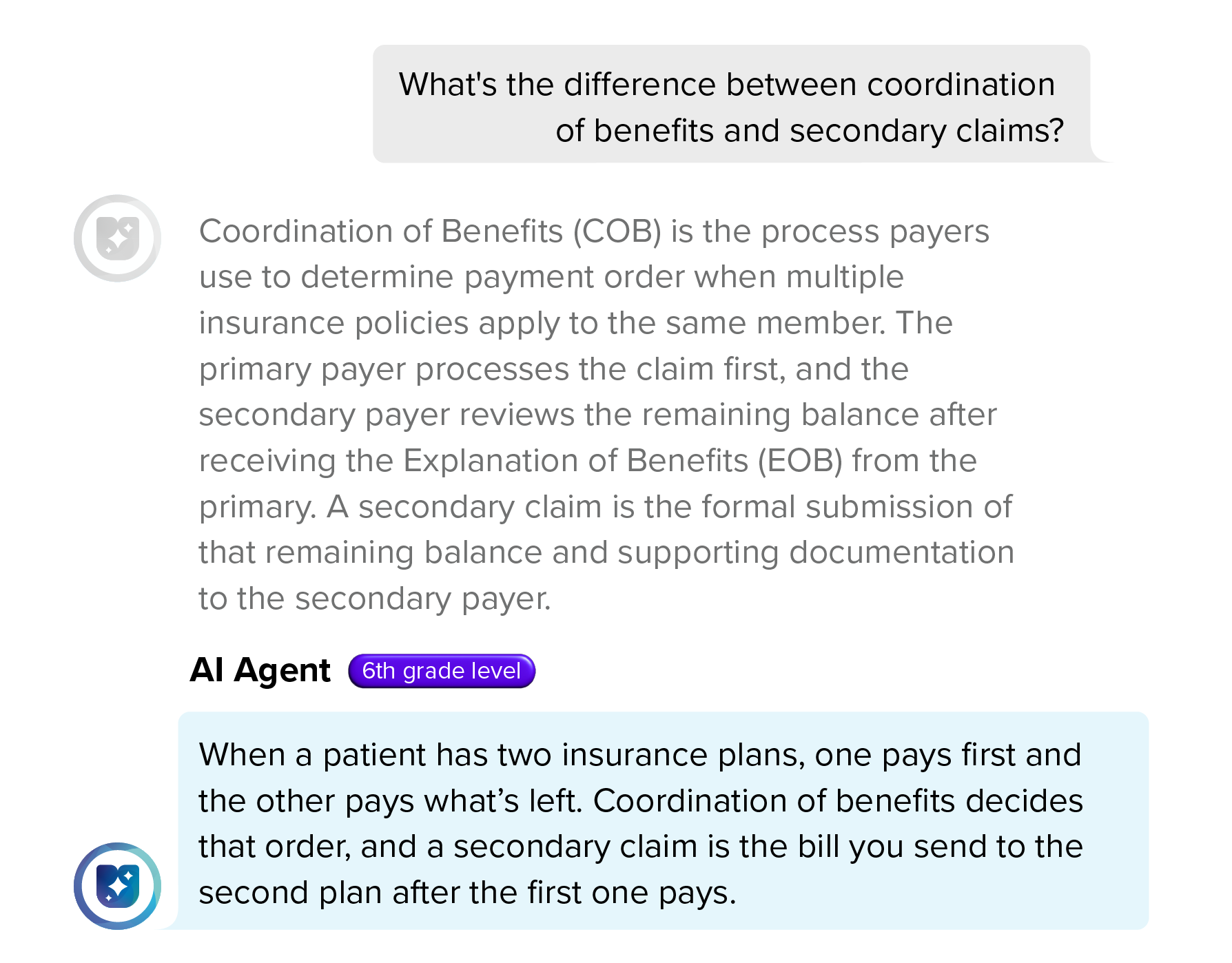
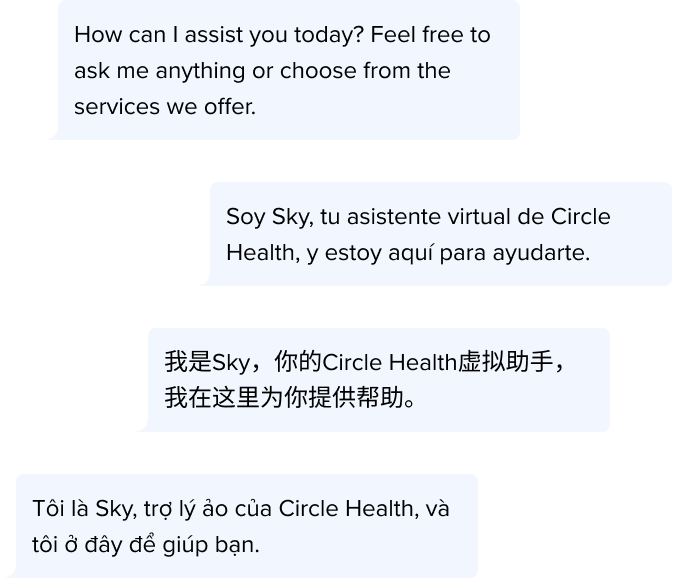
Delivers WCAG-compliant, multilingual experiences that simplify usage for all audiences and abilities.
Automate Critical Provider Service Touchpoints
Outcomes That Matter
Resolve Inquiry Overload
Reduce inbound volume while uniting benefit and coverage data across channels for accurate, instant answers.
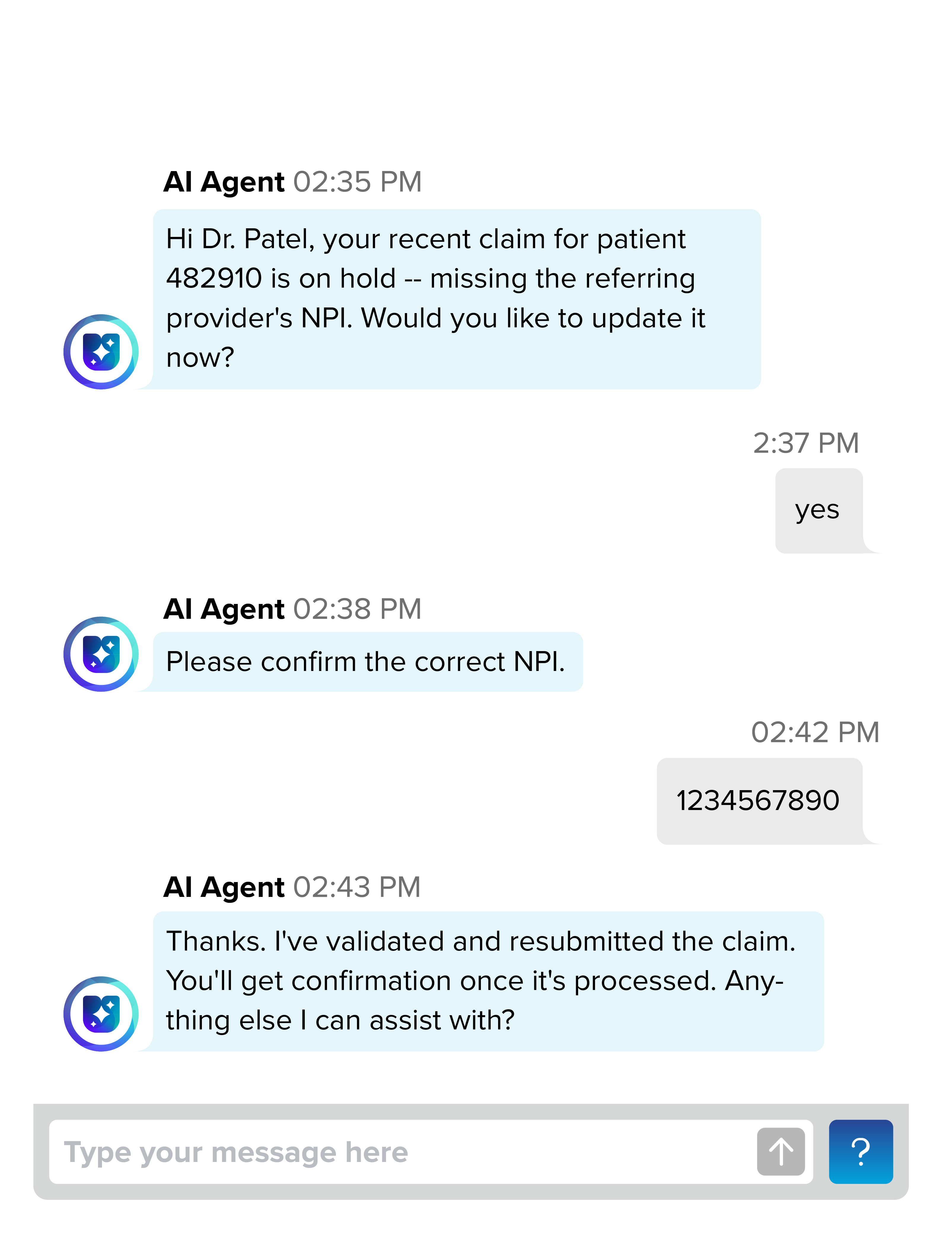
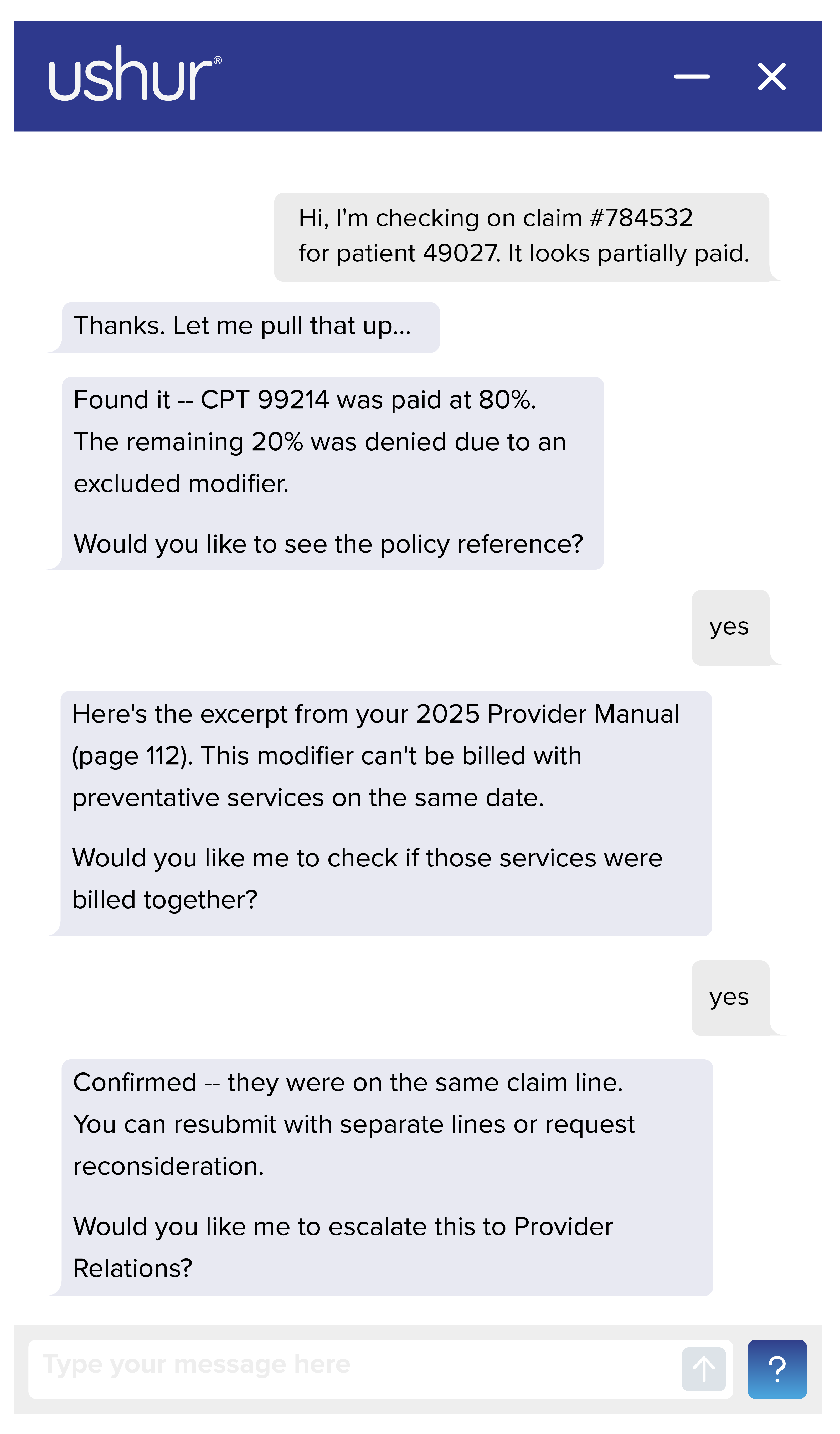
Faster Payments and Resolutions
Deliver immediate billing clarity and guided next steps that shorten payment cycles and speed up claim resolutions.
Stronger Provider Relationships
Boost satisfaction scores through faster, frictionless proof-of-coverage and document handling experiences.
Accelerated Adjudication and Onboarding
Streamline claim and credentialing workflows to cut cycle times and strengthen provider network stability.
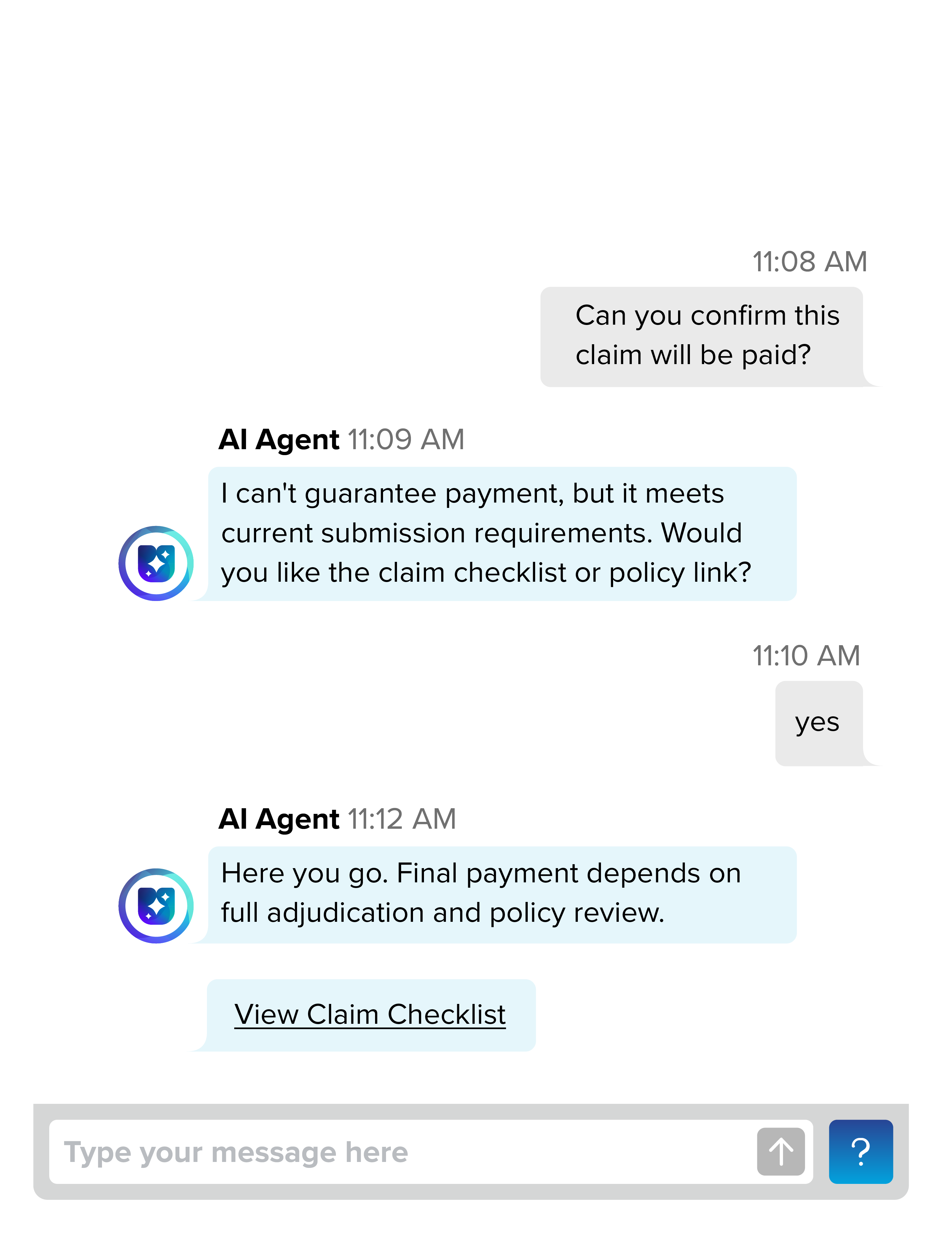
Accurate Data, Confident Decisions
Ensure every interaction reflects precise, contract-honoring data that improves compliance and reduces rework.
Always-On Scalability
Maintain consistent service quality during surges, spikes and after-hours demand with reliable 24/7 performance.
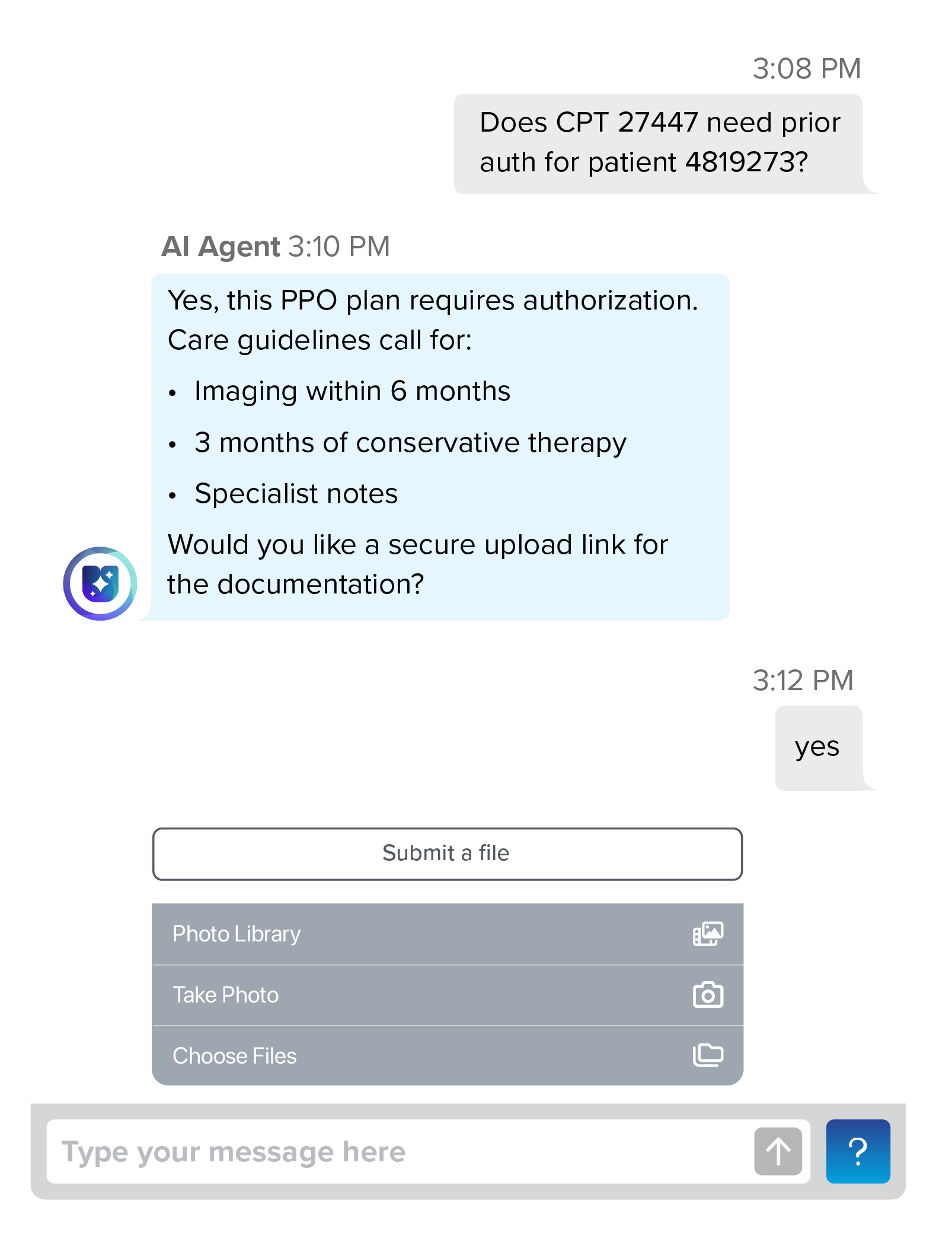
Intelligent, Personalized Support — Anytime. Anywhere.
Leverage real-time data, payer-specific insights and proactive recommendations to deliver 24/7 support. Tailor guidance to each provider by contextualizing their contract and delivering clear, actionable next steps.
Ready out of the box
Knowledge
Accesses provider agreements, claims records, and provider directories to deliver fast, context-rich answers that reduce manual lookups and improve accuracy.
Converse
Engages providers through secure and compliant conversations that collect missing information, clarify requests, and confirm next steps automatically.
Summarize
Translates complex authorizations, claim decisions, and policy details into clear and actionable summaries that reduce confusion and follow-ups.
Reach providers wherever they are — with confidence and peace of mind
Safeguarded by industry-specific protocols to keep every interaction compliant and secure.













Trusted by leading healthcare companies
A Large California Health Plan Automates Provider Support with AI Agents
- Deflect high-volume calls by automating benefits, claims, and credentialing inquiries through digital self-service.
- Reduce administrative costs by cutting the cost-to-serve on repetitive provider questions.
- Accelerate provider workflows by delivering instant, accurate responses that help providers move faster on behalf of patients.
.png)