.png)
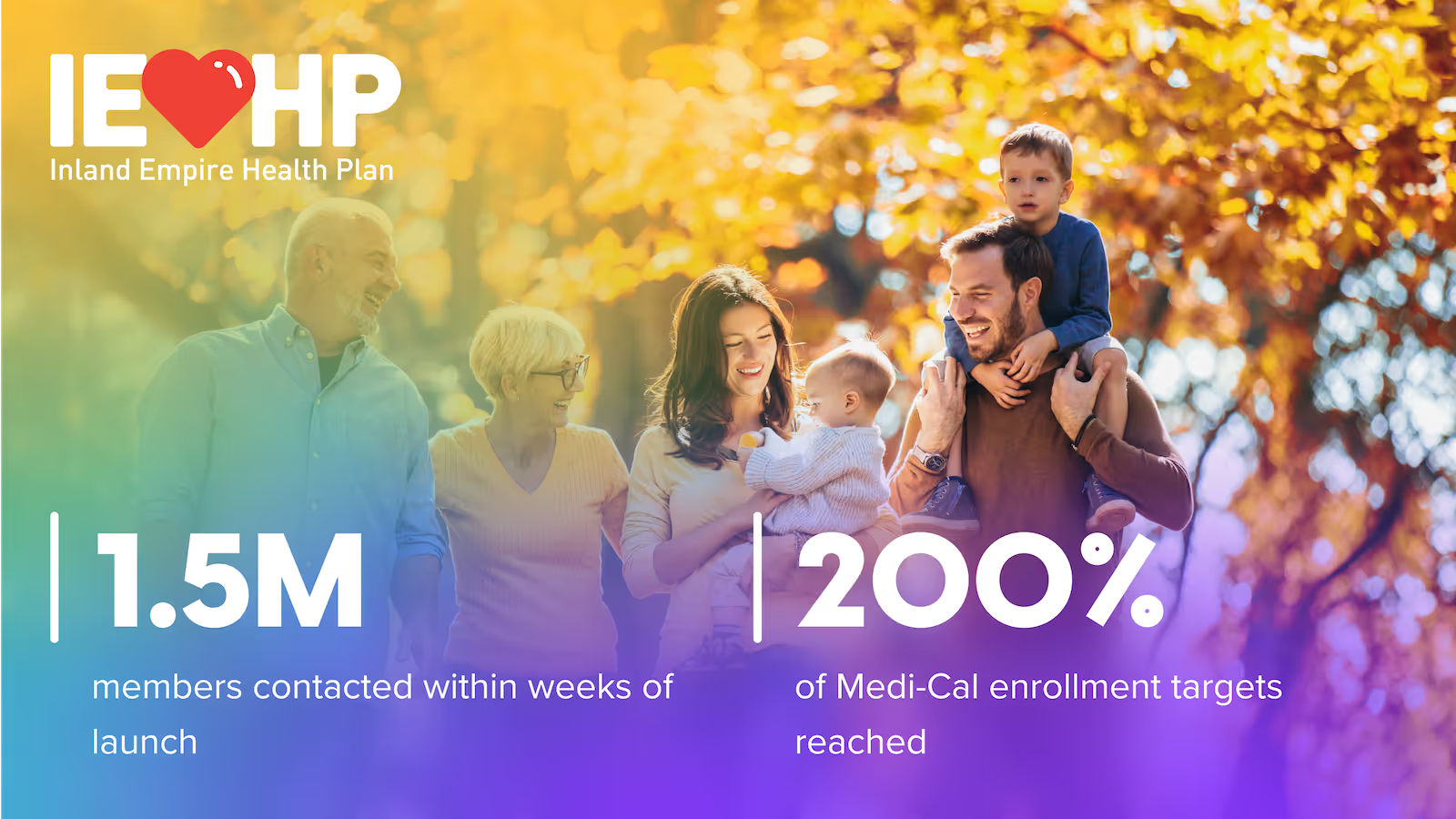
Ushur for Medicaid
Transform Medicaid Member Experiences & Cost Efficiency
Meet rising expectations with HIPAA-secure, multilingual automation that simplifies redetermination, reduces call volumes, and keeps vulnerable members covered.
Solving Medicaid Health Plans’ Most Persistent Pain Points
Meet member needs at scale
Improve reach and engagement with proactive, multilingual digital experiences and 24x7 digital support while staying compliant.
Protect costs
Retain members at risk of procedural disenrollment, reduce high cost events and drive operational efficiency.
Improve health outcomes
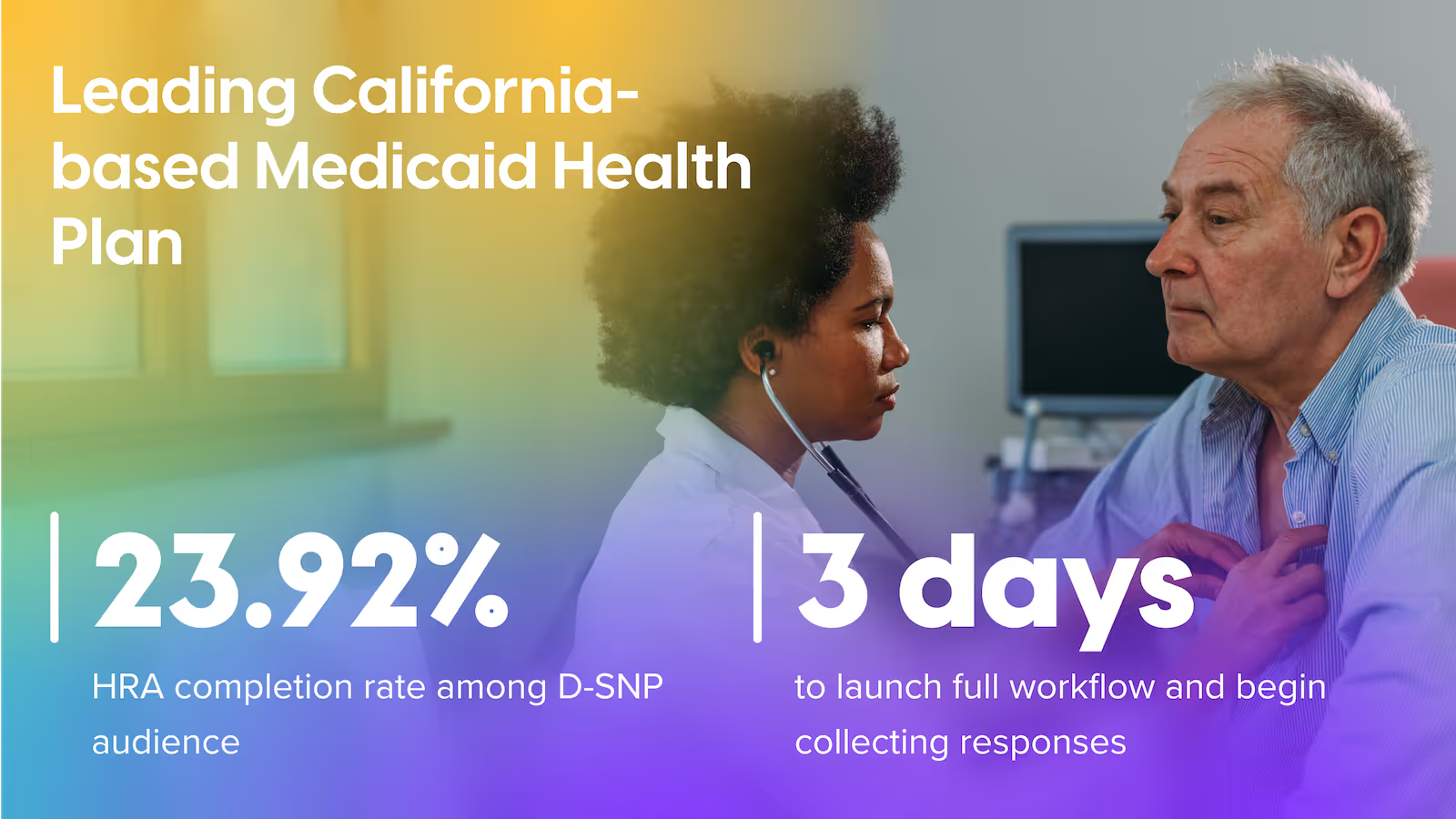
Medicaid members often face greater barriers to care. HIPAA-secure guided flows for HRA, SDOH, care navigation, and medication adherence improve HEDIS performance and close gaps in care.
Pre-built, Agentic AI solutions for Medicaid MCOs
AI Agent for Member Service
Virtual agent delivers instant answers and automating top asks, cutting call volume.
Medicaid Redetermination
Digital renewals retain coverage, eliminate paperwork and churn.
Chronic Conditions
Proactive monitoring lowers ER readmissions, improves chronic outcomes.
Medication Adherence
Smart refill reminders and barrier triage raise PDC 10-20 pts.
Maternal & Newborn Health
Prenatal-to-postpartum guidance reduces complications and NICU costs.
Medicaid Quality Engagement
SDOH surveys boost engagement, elevate Medicaid quality metrics.
Warm Welcome
Digital onboarding builds trust and drives early engagement.
Care Gap Closure
Smart nudges close care gaps and boost quality scores.
Drive higher ROI across your organization
Combine solutions and drive increased savings and revenue with Ushur AI Agents and Automation solutions designed for Medicaid use cases.
35,100 FTE Hours Saved Annually
Get in touch and see how we can help reduce member churn and increase dollars saved.
How Ushur delivers ROI
Trust Built-In
Rest assured the proper protocols are in place to keep every interaction compliant and secure.