Ushur for Medicare
Reduce Cost. Raise Star Ratings. Elevate Member Health.
From enrollment to care management, Ushur helps you drive healthier outcomes and higher Star Ratings with personalized, proactive, and compliant engagement at scale.
Solving Medicare Health Plans’ Most Persistent Pain Points
Star Ratings Performance
Proactively engage members with personalized outreach that closes care gaps, improves satisfaction, and drives higher quality scores.
Better Health Outcomes
Identify at-risk members, address barriers to care, reduce high cost events and guide them to take timely action that leads to healthier lives.
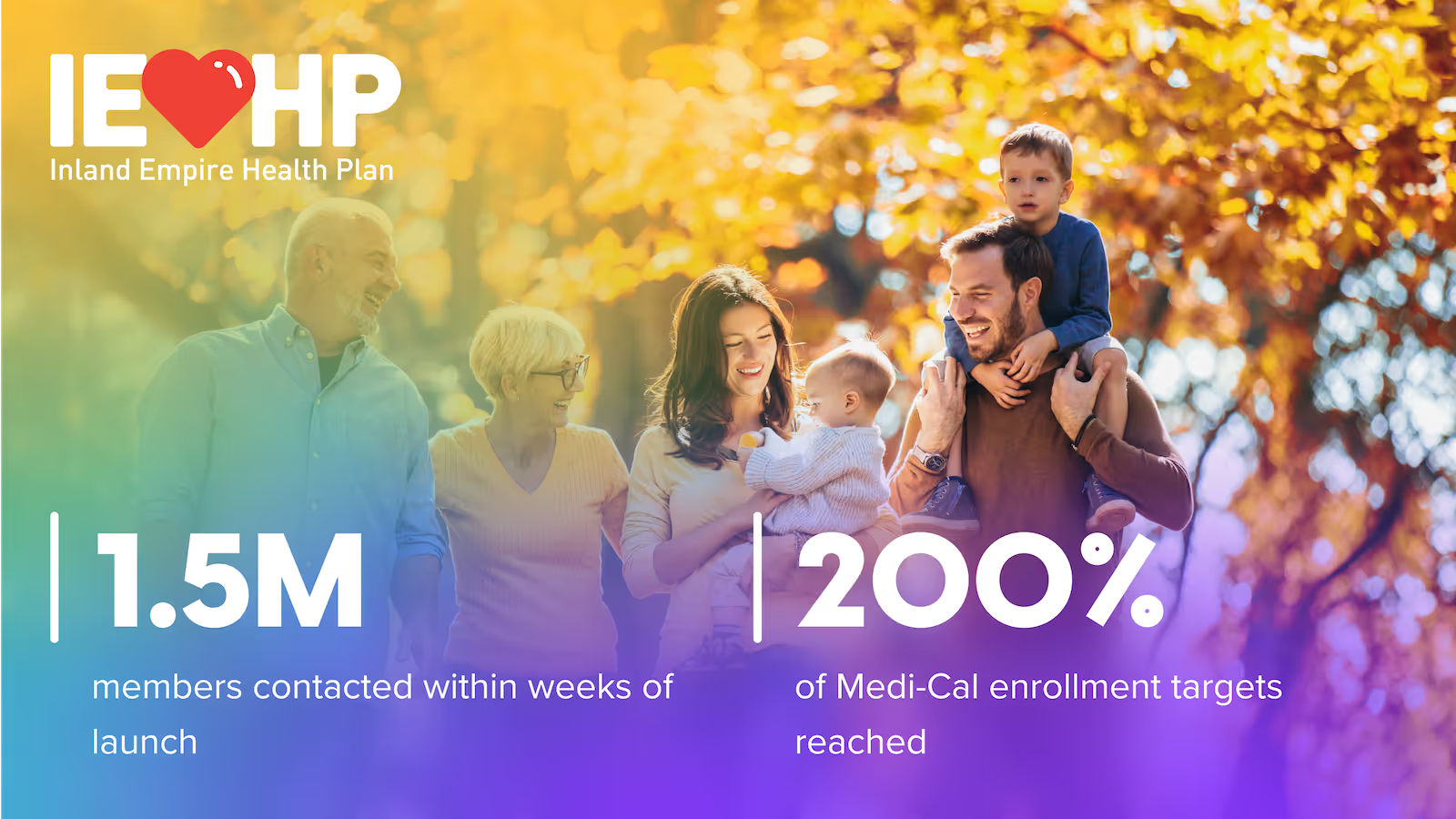
Gain & Retain Members
Simplify enrollment, boost benefit understanding and improve member satisfaction to protect growth and loyalty.

Pre-built, Agentic AI solutions for Medicare Plans
Member Service
Virtual agent delivers instant answers and automating top asks, cutting call volume.
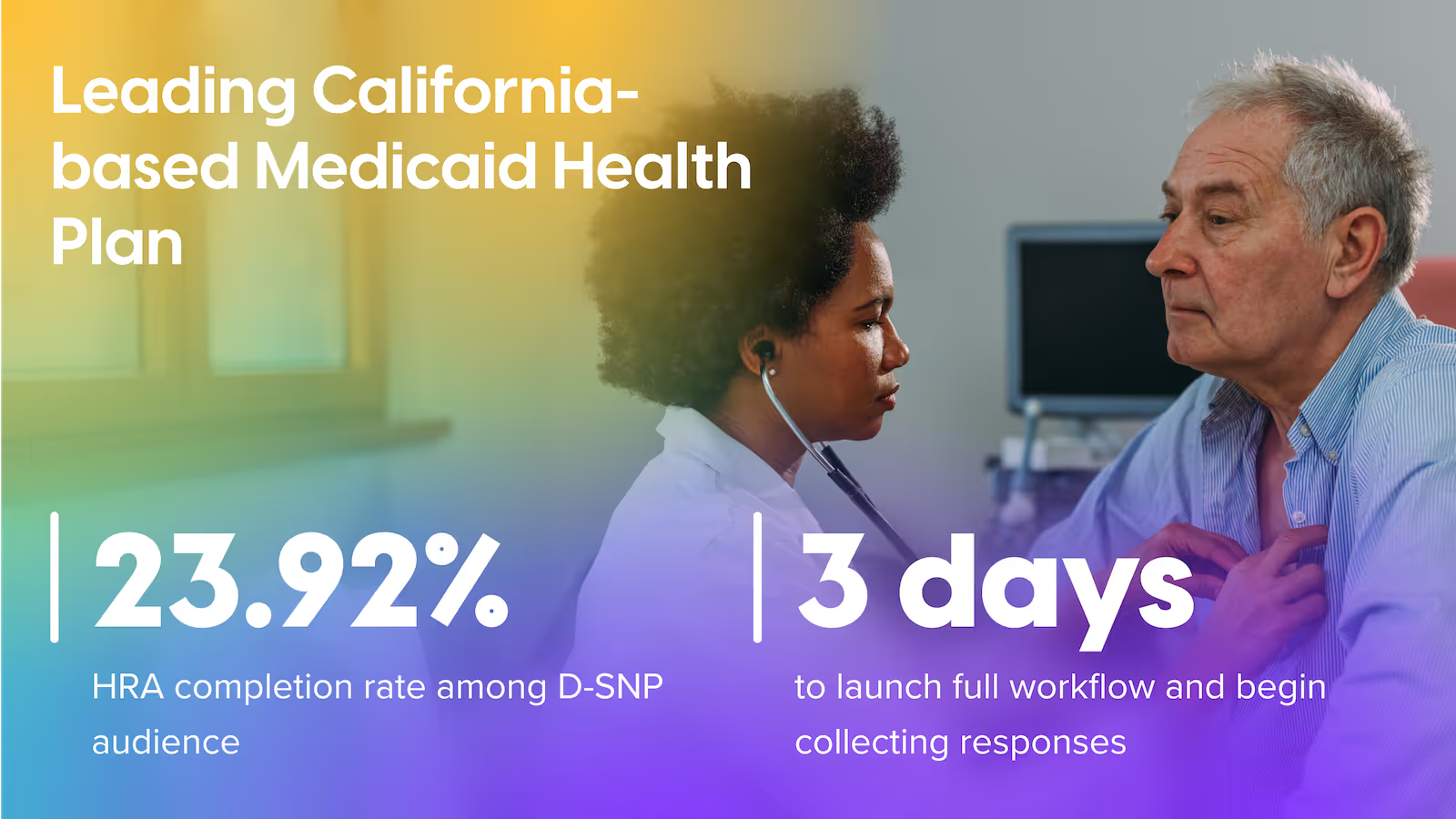
Population Health & Wellness
Pushes HRA, SDoH & preventive-care nudges that lift HEDIS and Star measures.
Chronic Conditions
Proactive digital coaching curbs ER visits for diabetes, hypertension, cardiac & MSK.
Medication Adherence
Smart refill reminders and barrier triage raise PDC 10-20 pts.
Warm Welcome
Digital onboarding builds trust and drives early engagement.
Care Gap Closure
Smart nudges close care gaps and boost quality scores.
Drive higher ROI across your organization
Combine solutions and see increased savings, better Star scores, and higher member satisfaction — all from one secure Ushur platform.
Get in touch and see how we can help reduce member churn and increase dollars saved.
How Ushur delivers ROI
Trust Built-In
Rest assured the proper protocols are in place to keep every interaction compliant and secure.